By Vincent Straub, Research Fellow (Centre for Policy Research on Men and Boys)
Half of us will experience a urological condition in our lifetime — yet awareness remains low.
Key facts at a glance
- 1 in 2 people will experience a urological condition in their lifetime.
- 10% of all daily medical care involves urology.
- 25 million Europeans (16% of people aged 40+) live with urinary incontinence.
- Prostate cancer is now the most commonly diagnosed cancer in the UK.
- 1 in 8 men in the UK will be affected by prostate cancer during their lifetime.
- Black British men are twice as likely to die of prostate cancer as white British men.
September marks Urology Awareness Month in the UK and European Urology Awareness Week (22–26 September) across Europe. Both campaigns aim to raise understanding of urological diseases — conditions affecting the urinary system and male reproductive organs.
The word urology comes from the ancient Greek ouron (οὖρον), meaning urine, and the suffix -logia (-λογία), meaning the study of. Today, urology covers a vast area of medicine: from urinary tract infections and incontinence, to kidney stones, sexual health, infertility, and cancers of the urinary and reproductive organs.
Despite their prevalence, urological diseases often remain taboo topics, leading to delayed diagnosis and treatment, avoidable suffering, and higher health costs.
Why urology matters
- Life expectancy gains bring new challenges: more men and women are living longer with complex, costly urological health needs.
- Urological conditions affect both sexes, but men face particular risks from prostate, bladder, and testicular cancers, as well as fertility and sexual health issues.
- Prostate cancer has become the most common cancer in the UK
Prostate cancer: the leading urological cancer
Prostate cancer affects around 1 in 8 men in the UK during their lifetime (Urology Foundation). While many cases are slow-growing, others are aggressive and life-threatening if diagnosed late.
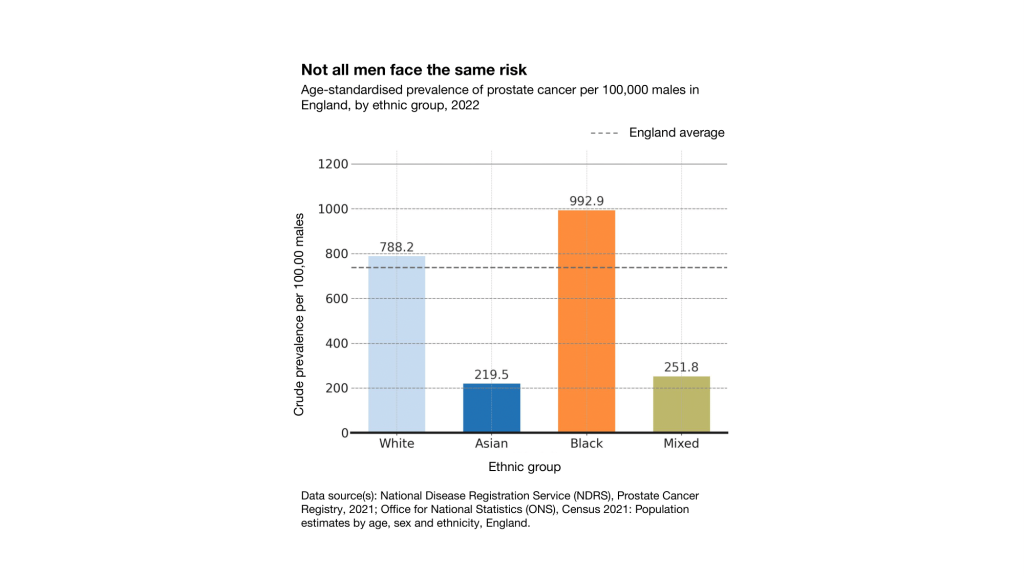
Importantly, not all men face the same risks. Ethnicity, age, genetics, and wider social factors all interact to shape outcomes (Dee et al., 2025). Recent registry data reveal stark inequalities: using case counts from the National Disease Registration Service (2021) and denominators from the Census 2021, crude prevalence per 100,000 males is significantly higher among Black men compared with other ethnic groups.
This underlines the need for an intersectional approach to awareness, prevention, and treatment — recognising how biology, ethnicity, and socioeconomic context overlap to drive disparities.
Research gaps and policy implications
Important gaps remain in understanding urological and reproductive health. Black men’s higher prostate cancer risk is still poorly explained, as most genetic studies over-represent White populations. The interplay between mental health, fertility and urological symptoms is under-researched (Straub et al., 2025), and the effects of alcohol, smoking and drug use on men’s reproductive health require further investigation (Lo et al., 2024).
Outcomes also differ sharply by ethnicity, age and deprivation, yet men are too often studied as a single group. Policymakers can help close these gaps by backing targeted awareness campaigns (especially for Black men), ensuring equitable access to early detection and treatment, and investing in inclusive research that connects genetics, behaviour, mental health and inequality.
Thankfully, new initiatives such as Prostate Cancer UK’s TRANSFORM trial, the biggest prostate cancer screening trial in 20 years, offer real promise — showing how research, policy and practice can come together to improve outcomes and reduce inequalities in men’s urological health.
Where to find out more
- Patients & the public: European Association of Urology patient hub
- Policymakers: All-Party Parliamentary Group on Prostate Cancer — Reducing the Risks report
- Healthcare providers: Prostate Cancer UK — primary care risk awareness
- Researchers & funders: The TRANSFORM trial, evaluating new approaches to screening
Note: Values in the figure are crude prevalence rates per 100,000 males, calculated using NDRS prostate cancer case counts and ONS Census 2021 denominators. Rates are not age-standardised; true disparities may be underestimated, as Black and Asian populations are younger on average than the White population.
References
The Urology Foundation. Urology Awareness Month 2025. Available at: https://www.theurologyfoundation.org/impact-achievements/campaigns/urology-awareness-month/ (Accessed 21 September 2025).
Dee, E.C., Todd, R., Ng, K. et al. Racial disparities in prostate cancer in the UK and the USA: similarities, differences and steps forwards. Nat Rev Urol 22, 223–234 (2025). https://doi.org/10.1038/s41585-024-00948-x
Straub, V.J., Mills, M.C. The interplay between male fertility, mental health and sexual function. Nat Rev Urol 22, 1–2 (2025). https://doi.org/10.1038/s41585-024-00936-1
Lo, J.O., Hedges, J.C., Chou, W.H. et al. Influence of substance use on male reproductive health and offspring outcomes. Nat Rev Urol 21, 534–564 (2024). https://doi.org/10.1038/s41585-024-00868-w